Connect With Us
Blog
Items filtered by date: July 2024
Ankle Sprains and Degrees of Injury

An ankle sprain occurs when ligaments, tough bands of tissue that connect bones, are stretched or torn due to excessive twisting or rolling of the ankle. This injury typically occurs during physical activities or sudden movements that stress the joint beyond its normal range of motion. There are three degrees of ankle sprains, each varying in severity. A mild sprain involves slight stretching and microscopic tearing of ligaments, causing mild pain and swelling. A moderate sprain includes partial tearing of ligament fibers, resulting in more significant pain, swelling, and difficulty walking. A severe sprain indicates a complete tear, or rupture, of ligaments that leads to intense pain, swelling, bruising, and instability in the ankle joint. Proper diagnosis and treatment, which may include rest and compression are vital for recovery and preventing long-term complications. If you have sprained your ankle, it is suggested that you consult a podiatrist who can successfully treat this condition.
Ankle sprains are common but need immediate attention. If you need your feet checked, contact Dr. Royall from Mountain View Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
How Does an Ankle Sprain Occur?
Ankle sprains take place when the ligaments in your ankle are torn or stretched beyond their limits. There are multiple ways that the ankle can become injured, including twisting or rolling over onto your ankle, putting undue stress on it, or causing trauma to the ankle itself.
What Are the Symptoms?
- Mild to moderate bruising
- Limited mobility
- Swelling
- Discoloration of the skin (depending on severity)
Preventing a Sprain
- Wearing appropriate shoes for the occasion
- Stretching before exercises and sports
- Knowing your limits
Treatment of a Sprain
Treatment of a sprain depends on the severity. Many times, people are told to rest and remain off their feet completely, while others are given an air cast. If the sprain is very severe, surgery may be required.
If you have suffered an ankle sprain previously, you may want to consider additional support such as a brace and regular exercises to strengthen the ankle.
If you have any questions please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Are Bunions Affecting Your Everyday Life?
Osteoarthritis of the Big Toe

Osteoarthritis, a degenerative joint disease commonly associated with aging, can affect any joint in the body, including the big toe. When osteoarthritis strikes the big toe, it leads to pain, stiffness, and reduced mobility, impacting daily activities such as walking and standing. Unlike rheumatoid arthritis, which is an autoimmune disorder, osteoarthritis of the big toe is primarily caused by wear and tear on the joint cartilage over time. Factors like genetics, previous injuries, and excessive stress on the joint can also contribute to its development. Individuals with occupations or hobbies that involve repetitive movements or excessive pressure on the feet are at a higher risk. Early symptoms may include discomfort and swelling around the joint, which can progress to chronic pain and deformity if left untreated. Management strategies for osteoarthritis of the big toe include lifestyle modifications, pain management techniques, orthotic devices, and in severe cases, surgical intervention to repair or replace the damaged joint. If you are experiencing any stiffness in your foot specifically the big toe, it is urged that you consult a podiatrist who can accurately diagnose and provide you with the foot care you need.
Arthritis can be a difficult condition to live with. If you are seeking treatment, contact Dr. Royall from Mountain View Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
Arthritic Foot Care
Arthritis is a term that is commonly used to describe joint pain. The condition itself can occur to anyone of any age, race, or gender, and there are over 100 types of it. Nevertheless, arthritis is more commonly found in women compared to men, and it is also more prevalent in those who are overweight. The causes of arthritis vary depending on which type of arthritis you have. Osteoarthritis for example, is often caused by injury, while rheumatoid arthritis is caused by a misdirected immune system.
Symptoms
- Swelling
- Pain
- Stiffness
- Decreased Range of Motion
Arthritic symptoms range in severity, and they may come and go. Some symptoms stay the same for several years but could potentially get worse with time. Severe cases of arthritis can prevent its sufferers from performing daily activities and make walking difficult.
Risk Factors
- Occupation – Occupations requiring repetitive knee movements have been linked to osteoarthritis
- Obesity – Excess weight can contribute to osteoarthritis development
- Infection – Microbial agents can infect the joints and trigger arthritis
- Joint Injuries – Damage to joints may lead to osteoarthritis
- Age – Risk increases with age
- Gender –Most types are more common in women
- Genetics – Arthritis can be hereditary
If you suspect your arthritis is affecting your feet, it is crucial that you see a podiatrist immediately. Your doctor will be able to address your specific case and help you decide which treatment method is best for you.
If you have any questions, please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Dealing With Morton’s Neuroma
 Morton's neuroma is a painful condition that affects the ball of your foot, usually between the third and fourth toes. This common issue is caused by the thickening of the tissue around one of the nerves leading to your toes. Thickening often occurs from excessive pressure or irritation from wearing tight or high-heeled shoes. Activities that involve repetitive foot stress, like running or certain sports, can also advance the development of Morton's neuroma. Morton's neuroma can significantly impact your ability to walk comfortably. As the tissue around the nerve thickens, it causes sharp, burning pain in the ball of your foot, which can make each step excruciating. The pain often spreads into your toes, causing numbness or a tingling feeling. Over time, walking or even standing for a long time can become hard, making it tough to complete daily activities and move around normally. The discomfort can also cause you to alter your walking pattern to avoid putting pressure on the painful area. This might lead to additional problems in areas such as the knee, hip, or back due to the uneven balance of weight. If you are struggling with Morton’s neuroma, it is highly suggested you consult with a podiatrist for an exam and diagnosis, followed by treatment options.
Morton's neuroma is a painful condition that affects the ball of your foot, usually between the third and fourth toes. This common issue is caused by the thickening of the tissue around one of the nerves leading to your toes. Thickening often occurs from excessive pressure or irritation from wearing tight or high-heeled shoes. Activities that involve repetitive foot stress, like running or certain sports, can also advance the development of Morton's neuroma. Morton's neuroma can significantly impact your ability to walk comfortably. As the tissue around the nerve thickens, it causes sharp, burning pain in the ball of your foot, which can make each step excruciating. The pain often spreads into your toes, causing numbness or a tingling feeling. Over time, walking or even standing for a long time can become hard, making it tough to complete daily activities and move around normally. The discomfort can also cause you to alter your walking pattern to avoid putting pressure on the painful area. This might lead to additional problems in areas such as the knee, hip, or back due to the uneven balance of weight. If you are struggling with Morton’s neuroma, it is highly suggested you consult with a podiatrist for an exam and diagnosis, followed by treatment options.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Royall of Mountain View Foot & Ankle Clinic. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Facts About Plantar Fasciitis and Its Symptoms
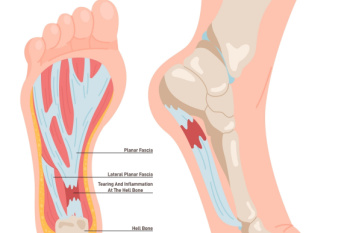
Plantar fasciitis is a common cause of heel pain, resulting from inflammation of the plantar fascia, which is the thick band of tissue that runs along the bottom of the foot and connects the heel bone to the toes. The condition typically causes a sharp, stabbing pain in the heel, particularly noticeable with the first steps in the morning or after periods of inactivity. Risk factors include prolonged standing, high-impact activities, obesity, and wearing unsupportive shoes. The pain usually lessens with movement but can return after long periods of standing or sitting. Treatment often involves stretching exercises, wearing proper footwear, and rest to reduce inflammation. In severe cases, orthotics or injections may be necessary. Plantar fasciitis can cause severe pain and can hinder completing daily activities. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can accurately diagnose and treat plantar fasciitis.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Royall from Mountain View Foot & Ankle Clinic. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What are Pressure Ulcers on the Feet and Ankles?
 Pressure ulcers on the feet and ankles, also known as pressure sores or bedsores, are injuries to the skin and underlying tissue resulting from prolonged pressure. These ulcers are common in individuals with limited mobility, and can often affect the feet. Intrinsic factors, such as poor nutrition, age, and medical conditions like diabetes, affect the body's ability to heal and withstand pressure. Extrinsic factors involve external forces like friction and prolonged pressure from staying in one position. Symptoms include redness, pain, and open sores, which can progress to deep wounds exposing muscle and bone. Pressure ulcers occur due to reduced blood flow to the affected area, leading to tissue damage. Prevention includes regularly changing positions, using supportive devices, maintaining good nutrition, and keeping the skin clean and dry. Treatment involves relieving pressure, cleaning wounds, and using dressings or medications to promote healing. Advanced cases might require surgical intervention. If you are suffering from a pressure ulcer on your feet or ankles, it is suggested that you schedule an appointment with a podiatrist as soon as possible for care.
Pressure ulcers on the feet and ankles, also known as pressure sores or bedsores, are injuries to the skin and underlying tissue resulting from prolonged pressure. These ulcers are common in individuals with limited mobility, and can often affect the feet. Intrinsic factors, such as poor nutrition, age, and medical conditions like diabetes, affect the body's ability to heal and withstand pressure. Extrinsic factors involve external forces like friction and prolonged pressure from staying in one position. Symptoms include redness, pain, and open sores, which can progress to deep wounds exposing muscle and bone. Pressure ulcers occur due to reduced blood flow to the affected area, leading to tissue damage. Prevention includes regularly changing positions, using supportive devices, maintaining good nutrition, and keeping the skin clean and dry. Treatment involves relieving pressure, cleaning wounds, and using dressings or medications to promote healing. Advanced cases might require surgical intervention. If you are suffering from a pressure ulcer on your feet or ankles, it is suggested that you schedule an appointment with a podiatrist as soon as possible for care.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Royall from Mountain View Foot & Ankle Clinic. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Lehi, UT . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blog Archives
- March 2025
- February 2025
- January 2025
- December 2024
- November 2024
- October 2024
- September 2024
- August 2024
- July 2024
- June 2024
- May 2024
- April 2024
- March 2024
- February 2024
- January 2024
- December 2023
- November 2023
- October 2023
- September 2023
- August 2023
- July 2023
- June 2023
- May 2023
- April 2023
- March 2023
- February 2023
- January 2023
- December 2022
- November 2022
- October 2022
- September 2022
- August 2022
- July 2022
- June 2022
- May 2022
- April 2022
- March 2022
- February 2022
- January 2022
- December 2021
- November 2021
- October 2021
- September 2021
- August 2021
- July 2021
- June 2021
- May 2021
- April 2021
- March 2021
- February 2021
- January 2021
- December 2020
- November 2020
- October 2020

